Physioanswers.com has a great article explaining why physical therapy is worth the investment. I have added the text from the article below, but you can see the article for yourself here: http://www.physioanswers.com/2014/01/why-physical-therapy-is-worth-paying.html
"It’s inevitable: the year comes to a close and the exodus of patients leaving from physical therapy starts. Just this year alone we had close to 15 to 20 patients opt out of finishing their therapy. Why?
A few may be close to discharge and find the start of a new year as an opportunity to take things on themselves. I fully support that choice! However, many of my patients cite the reason they are stopping therapy is due to the fact that “Insurance won’t cover them anymore”. While this isn’t entirely true, the truth is that a new year often means meeting a new deductible – and if you hadn’t noticed yet, deductibles are not getting lower. The average patient in my clinic has to meet a $1000-$2000 deductible prior to any insurance coverage and then often are covered at 80% beyond that. I can understand why patients are struggling to stay with PT. That’s a huge chunk of change not everyone has available to dish out. However, I write this article bearing in mind that most people end up meeting their deductible at some point during the year. Ultimately, as conscious consumers you will choose to spend your health care dollars in the place of best value and highest return on investment. I will argue that PT is one of, if not the best place to put money toward your deductible.
1. Physical Therapy (PT) is cheap. Almost to a flaw. Now before you balk at this idea bear in mind the rest of the medical world out there. A trip to a PT roughly costs $100 a session (average). A trip to an orthopedic doctor, pain specialist, or other such professional will cost you roughly $150 for the consultation + more if further tests or imaging is ordered. What if medication is prescribed or injections are performed? Have you seen the price of medications today? And with those professionals what most often happens? A referral to PT. This not only pushes the start date to rehab further back, but also take precious time up (maybe away from work or kid)s. Speaking of time…
2. PTs take their time. Really. Value to most patients is what they get from an encounter with a medical professional. Lets break down a trip to a medical professional first (for ease I will use an orthopedic specialist but please reference your favorite): 30 minute drive. 15-120 minute wait prior to seeing doctor (no joke I’ve had patients wait 2 hours for a doctor). 5-15 minute consultation. 30 minute imaging. 10 minute check out. 30 minute drive home. Go home with meds: 30 minute fill up. Referral for PT. Follow up in 30 -60 days. Or not at all. Upwards of 4 hours invested on the long end.
Cost: $150 for consultation, $150 for imaging, $20 for medication. $320 towards your deductible.
Now lets look at PT. (SIDE NOTE: in almost every state PT is open access meaning you do not need a referral from a physician prior to treatment). 30 minute drive. 5-15 minute wait to see PT (if that). 60 minute consultation: this includes hands on treatment, supervised exercise routines, pain control techniques, in depth education on condition. Go home with strategies for pain control, corrective exercises, home program. Follow up in 2-7 days.
Cost: $100. A little over 2 hours invested.
It’s simple math. With PT you get more for less.
What are some other benefits you ask?!
3. PTs are trained in differential diagnosis. We’ve gone through 7 years of high level training including dissection of a cadaver and differential diagnosis classes as well as pharmacy courses, radiologic imaging courses and have significant hands on training during our schooling. We are movement specialists. Want to know if you have a torn rotator cuff? We have tests for that. Shoulder impingement? We have tests for that. Herniated disc? We have tests for that. Inner ear versus peripheral vertigo? We have tests for that. If your condition isn’t appropriate to physical therapy – we have the resources and knowledge to point you in the right direction at a much lower cost than your general practitioner or a specialist.
4. Our skill set is large. Physical therapists treat anything from vertigo to low back pain to incontinence to visual tracking dysfunction to lung clearing techniques. We use dry needling, spinal manipulation, belted mobilizations, soft tissue tools, active release technique, kinesiotaping as well as electric and ultrasound modalities (and much more) to get you better. More often than not the answer is yes, we treat that.
5. PT is becoming the Go-To profession of the medical world. Want an MRI? Go to a physical therapist first. Surgery? Go to a physical therapist first. In the military PTs are often the primary provider. Why? Because more often than not most musculoskeletal problems are solved with physical therapy. More and more studies are coming out about the cost effectiveness of physical therapy. And outcomes with physical therapy continue to be shown years down the road. You not only get treated in the short term, you learn how to make yourself better in the future.
6. We are part of a preventative model. What is the famous quote… “An ounce of prevention is worth a pound of cure”? PTs are unlike any other profession in our ability to treat problems now but also to educate and steer you clear of trouble spots in the future. We are a wellness community which is dedicated to lifelong wellness, not just short term fixes. You get to know us and we get to know you. You can’t really put a price on that.
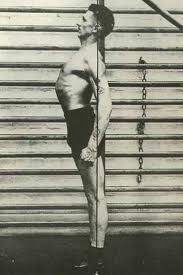
Something you may not know: you don’t have to be in pain to see a PT. Outcomes are better when you catch the problem early. Don't know if you have a problem? Get a movement screen just like you get your yearly checkup. Want to get in shape? PTs can put you on a safe and effective program- for almost the same cost as a personal trainer you get hands on care, body work if needed, appropriate exercises, a wide skill set and a commitment to prevention.
As the new year gets in full swing and you stride forward full of resolution steadfastness bear in mind the value you want to get from your health care dollars. I may be biased, but in my mind there is no better value than a physical therapist."
Contributed by Dr. Eric Christensen
This article is spot-on in quickly explaining why it's not always worth running around to physicians and having significant testing done, especially if it's not clear why you're having the symptoms you're experiencing. Physical therapy can not only typically fix the problem without any need to see a specialist, but if it does appear that you need to see another practitioner or physician, we can help steer your toward the proper person. We can also provide them information that we have gathered in our sessions with you to help them come to a diagnosis more quickly.
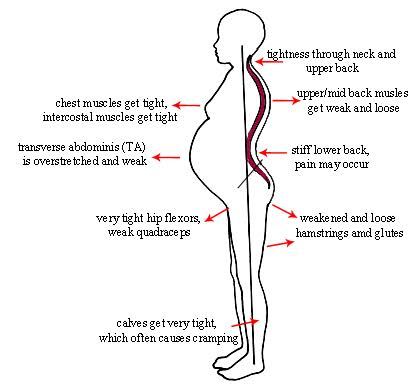
The doctors aren't sure what's causing your symptoms? Integrate 360 Physical Therapy is the right place for you! Many times there isn't a test or image that will show what is specifically causing your pain. There aren't enough white blood cells, joint inflammation, or pathologies present that can be picked up by these tests, but YOU ARE HAVING PAIN. Most of the time, our bodies are not moving efficiently and are causing muscle overuse, spasm, tendonitis, etc. This is what causes our pain, but it cannot always be picked up via blood test or image.
Tried physical therapy with no or minimal results? Integrate 360 is the place for you! Traditional physical therapy treats at, or closely around, the point of pain. For example, if you're having knee pain, a traditional therapist will evaluate your knee and then quickly screen your hip and ankle to see if they are complicating matters at all. Many times, this isn't thorough enough of an evaluation and the patient will experience less than optimal, or temporary results.
At Integrate 360, no matter what your symptoms are (vertigo, incontinence, back pain, shoulder injury, headaches, jaw pain, etc.), we look at your entire body/system. The body is all connected and must be working correctly in all areas in order to be symptom free. For example, if someone had an ankle injury and limited mobility because they never received physical therapy, it can absolutely effect their shoulder pain! If they have a compensated walking pattern or standing posture, their spine will not be properly aligned. When their spine is off, their ribcage is in the wrong position. This make it very difficult for the shoulder blade to sit in the correct position on the ribcage and will be inherently unstable. The shoulder blade is half of the shoulder joint (the other half being the arm bone), so if it's not stable, it becomes very hard to move one's shoulder using the correct musculature. When poor mechanics occur, pain develops.
Come see our therapists at Integrate 360 and let us save you time, money, and offer you better results than moving through the medical system or seeing a traditional physical therapist. Call us at 314-733-5000 or email Lesley@integrate360pt.com or Nancy@integrae360pt.com for more information.